|
— Testosterone —
A Critical Hormone for Men and Women
By
Jeffry S. Life, M.D., Ph.D. and Alan P. Mintz, M.D.
Cenegenics
Medical Institute
Las Vegas, Nevada
Men
and Testosterone
Testosterone is a hormone that has been intimately tied throughout time to a man’s virility
and sexuality. It is the major steroid hormone of the testicles. However, testosterone is much more than just a sex hormone.
With testosterone receptor sites in the brain and heart, and in fact throughout the entire body, testosterone plays a critical
role in maintaining a healthy immune system, insuring proper heart function, and regulating mood and cognition, controlling
blood sugars, regulating healthy cholesterol levels, controlling blood pressure, preventing heart attacks, and even reducing
the risk for prostate cancer.
Testosterone production in the male begins when the pituitary gland, located deep inside
the brain, secretes lutenizing hormone (LH), which in turn, stimulates the Leydig cells in the testicles to produce testosterone.
It is estimated that men are born with 700 million Leydig cells and they begin losing 6 million each year after their twentieth
birthday. In spite of these losses, studies have found that testosterone levels peak in men at about age 30. After this, testosterone
levels begin declining an average of 2% a year.
Declines in testosterone production are due to several factors besides
decreases in Leydig cell numbers. Diminished testicular response to pituitary signals that initiate testosterone production
and a poor coordination of the release of these pituitary signals play the most important role in testosterone decline. Another
reason for testosterone decline is because most of the testosterone that is secreted into the bloodstream attaches to a protein
called sex hormone binding globulin (SHBG). Testosterone that is not bound to SHBG is called free testosterone and it is only
in this form that testosterone can exert its powerful effects on all of the body’s cells. An increase of SHBG occurs
in many men as they age, especially if they are obese. As SHBG levels increase, the amount of testosterone that is available
to act on cells diminishes even further.
These age-related declines in total and free testosterone levels in men are
associated with easily identifiable, classic signs and symptoms called andropause. Andropause can cause significant problems
that include negative attitudes about life in general, a loss of focus and drive, a questioning of one’s values and
accomplishments, loss of goals and directions in life, decreased libido, depression, and even cognitive impairments. Declines
in sex drive, frequency of sexual thoughts, and erectile dysfunction are additional problems that are directly related to
falling levels of free testosterone and these can have a profoundly negative impact on the male psyche and relationships.
Physical changes also occur and are characterized by thinning hair, a decline in lean muscle tissue, and an increase
in body fat (particularly abdominal and pectoral fat). As muscle mass declines, strength declines and risk for falls and fractures
increases. A decrease in bone mass is another major problem associated with declining levels of testosterone. Osteoporosis
is not just a woman’s disease—up to 30% of men aged 60 and over become osteoporotic. One out of every six men
will fracture a hip at some point in their life as a result of decreased bone density. Declines in stamina and exertional
performance are also a direct result of inadequate levels of testosterone as are declines in mental skills, concentration,
and memory.
Testosterone can be converted, by enzymes, into other hormones. One of these enzymes is called 5-alpha
reductase. It is found in especially high concentrations in the prostate gland where it converts testosterone into dihydrotestosterone
(DHT). Another enzyme, called aromatase, is found in skin, brain, fat, and bone. Aromatase converts testosterone into estradiol,
the human form of estrogen. As men age, more of the testosterone they produce is converted into estradiol. When there is too
much estradiol it competes with testosterone and negative consequences develop. These include prostate cancer, heart disease,
and stroke. Abnormal increases of estradiol are caused by excess amounts of aromatase enzyme, impaired liver function (often
caused by excessive alcohol or certain drug interactions), obesity (which increases aromatase enzyme), and zinc deficiency
(zinc is a natural aromatase enzyme inhibitor). In addition to declining levels of testosterone and increasing levels of estradiol,
growth hormone, thyroid hormone, and DHEA levels fall during andropause. As these levels decline, profound changes occur with
growth and metabolism that affect men both physically and mentally and add to their testosterone deficiency problems.
Today
the signs and symptoms of andropause should not be accepted as an inevitable consequence of the aging process. By utilizing
bio-identical hormones and accurate monitoring techniques, replacement therapy is now possible. Hormone optimization programs
offered by Age Management Medicine physicians have rapidly moved into the forefront of preventive medical care and have greatly
contributed to the enhancement of quality of life as men and women age.
Women
and Testosterone
Testosterone may be well known as a hormone that has been tied to a man’s virility and
sexuality, but few realize that it is also a very important hormone for women. As women age, estradiol and progestin levels
begin falling as they enter menopause. Testosterone (produced in the ovaries and adrenal glands), thyroid hormone, and growth
hormone levels also decline during this time. As the levels of these key hormones diminish, profound degenerative changes
begin occurring with growth and metabolism that affect the breasts, vagina, bones, blood vessels, gastrointestinal tract,
urinary tract, cardiovascular system, skin, brain, and energy levels.
We now know testosterone is critically important
for a woman’s libido, sexual responsiveness, mood, and generalized feelings of well-being. Women, like men, also need
adequate testosterone levels for peak mental acuity and the maintenance of healthy bone density and muscle tissue. Maintaining
bone density is absolutely critical for women. Unsupplemented women have a 50% chance of experiencing a pathological fracture
of their hip or vertebra at some point in their life. This is a frightening statistic because a hip fracture carries with
it a 25% six-month mortality rate, and a 50% two-year mortality. Testosterone also plays a key role in the prevention of the
accumulation of unwanted body fat, heart disease, and loss of cognitive function in women. Testosterone replacement therapy
is now recommended for women with suboptimal blood levels. Like men, women must have all of their hormones at optimal levels
and be followed with laboratory studies on a regular basis after therapy is started.
Testosterone Measurement
Clinical signs and symptoms are important indicators that an individual
needs testosterone replacement therapy. However, objective laboratory measures must be obtained to properly institute and
manage therapy. These lab measurements are also necessary to rule out or address any accompanying medical problems. To adequately
measure testosterone levels, both total and free testosterone studies should be obtained. The normal laboratory ranges for
these is, ironically, the same for 20 year olds and 70 year olds
Obviously, the fifty-year span from age 20 through 70
with the same normal range is not a useful guide to determine optimal testosterone levels for older individuals. Typically
there is a 70% decline from the more youthful levels to the levels typically seen after age 40, and this will produce most,
if not all, of the problems associated with low testosterone levels described above. Yet a level this low does fall in this
broad range and is declared "within the normal range" by today’s laboratory standards. A more accurate approach would
be to use the upper third of the normal range for one’s age as the optimal or normal level.
The decision to institute
testosterone replacement therapy should always be made in the context of other hormonal and laboratory studies. Prostate Specific
Antigen (PSA) measurement and a digital rectal exam of all men must accompany testosterone blood levels at the time of the
initial evaluation to screen for any pre-existing prostate disease and they need to be followed at regular intervals. Other
studies, such as thyroid hormones, growth hormone (hGH), leutinizing hormone (LH), dehydroepiandrosterone (DHEA), estradiol,
progesterone, blood count, lipid profiles, and other laboratory and metabolic markers (such as body composition and bone density)
all play important roles in maximizing a testosterone replacement program in both men and women. Once therapy is initiated,
follow up hormone levels, as well as other markers, must be monitored over time at regularly scheduled intervals by a well-trained
physician to maximize success and assure safety.
Testosterone
Therapy
Any hormone therapy including testosterone therapy is very serious business and must be performed by
physicians trained in hormonal modulation. Before any testosterone supplementation program is started, all key hormone levels
must be evaluated and therapy should be based on the augmentation of all hormones with suboptimal levels. After the decision
has been made to optimize hormone levels, the next step is to decide on the best means of administration.
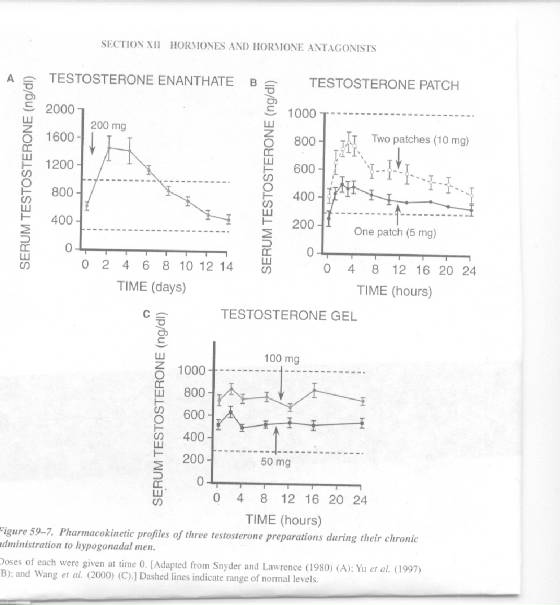
The best method
of testosterone delivery varies from individual to individual, and is dependent upon several factors. Optimally, a testosterone
delivery method should be clinically effective in correcting the signs and symptoms of testosterone decline and produce predictable
and reproducible optimal levels of testosterone without increasing levels of other potentially harmful hormones. The fact
that testosterone can be converted to estradiol by an aromatase enzyme is a serious concern for men because, in some, any
intervention that raises testosterone levels will raise estradiol levels. With proper laboratory follow up, this is easily
identified and corrected. The raising of serum levels of dihydrotestosterone (DHT) can also be clinically important in men.
DHT, as discussed earlier, is the hormone associated with male-pattern baldness and prostate enlargement. These do not become
a problem if DHT levels are closely monitored and controlled.
Testosterone is available directly in injectable, topical,
and implantable formulations, and may also be supplemented indirectly by the administration of human chorionic gonadotropin
(hCG). At present, there are no recommended oral testosterone formulations in the United States for men. Testosterone pellets
have been developed for men that can provide augmented serum testosterone levels for up to six months. Pellets, however, require
a surgical procedure for implantation and removal, and once they are placed they do not allow for altering dosages based on
an individual's testosterone blood levels.
An oral preparation
that is useful for helping normalize testosterone levels in women is DHEA. Men do not convert DHEA into meaningful levels
of testosterone, but many women do. A good first step in improving testosterone levels in women is to optimize DHEA levels
and then re-check testosterone levels after 5-7 weeks. If testosterone levels have not increased, direct testosterone therapy
can be started at that time.
Testosterone for
use in men is available in a formulation that provides a long biological effect time and can be purchased by prescription
in a low cost, easily self-injectable form. A dosage interval of once a week works very well. Delivering testosterone in this
way has a 100% success rate in providing every cell with usable hormone. It is also easy to precisely control the dosage of
testosterone and manage the results by following levels over time at regular intervals. This is the supplementation of choice
for men whose testicles are no longer able to produce testosterone in adequate amounts.
Testosterone formulations
are also available for topical placement, which allows testosterone to be absorbed through the skin. Testosterone cream is
the therapy of choice for raising testosterone levels in women. There is only limited application for topical testosterone
in men because this method can produce elevated serum levels of DHT. The very small amounts of testosterone cream required
to raise testosterone levels in women have not been associated with any problems. Testosterone patches are available by prescription
for men but have been associated with problems including, inability to achieve adequate serum testosterone levels and local
reactions from the adhesive. Mild to moderate reactions occur in as many as 50% of men using some formulations of the skin
patch. Patches have also been shown in studies to produce a 30-50% failure rate in clinical applications.
An interesting
new way of increasing testosterone levels in men has been achieved through the use of human chorionic gonadotropin (hCG).
hCG is a hormone that is able to bind to lutenizing hormone (LH) receptors with the same binding affinity as LH. Administration
of hCG can, therefore, mimic the same effect as LH and increase testosterone production by stimulating Leydig cells in the
testicles. In men who still have a functional LH/testosterone control loop, testosterone production with hCG is the most physiologic
method and is not associated with the testicular atrophy that can occasionally happen with direct testosterone administration.
The preferred method of administering hCG is to give self-administered subcutaneous doses with a tiny insulin syringe twice
weekly. With normal aging, the testicles will at some point stop responding to the LH and hCG signals. If testosterone levels
do not rise in a patient receiving hCG after 6 weeks, we know the "disconnect" between the testicles and the pituitary gland
has occurred and direct testosterone supplementation is the preferred route*.
Once a hormonal augmentation program is initiated,
laboratory markers, which include hormone blood levels, should be followed at regularly scheduled intervals and therapy must
be adjusted accordingly if an endocrine supplementation program is to be safe and effective. Physicians specifically trained
and certified in Age Management Medicine are best suited to oversee such programs.
Conclusion
Hormonal balance plays a huge role in determining the overall health and wellbeing
of both men and women. Today age-related hormone deficiencies and imbalances are correctable and optimal hormone balances,
that place individuals in the upper percentiles of their normal hormone ranges, can be safely achieved when performed by a
competent physician specifically trained and certified in Age Management Medicine. Men, women, and their loved ones need not
suffer the consequences of a mid-life crisis. There is definitely hope. It is now within our power to make the rest of our
lives the best of our lives!
References
are available on request.
*For
further information on testosterone supplementation and dosing see Dotson A. “Methods of Testosterone Supplementation
for Men and Women”. Cenegenics Testosterone Medical Information Gateway. 2004; www.testosterone-articles.com .
About
the Authors
Alan P. Mintz, M.D., is Chief Medical Officer, Chief Executive Officer, and Co-Founder, of Cenegenics
Medical Institute. He is a Diplomate for the American Board of Radiology, including Nuclear Medicine and Radiation Therapy
and is certified in Age Management Medicine. For further information contact Dr. Mintz or Dr. Life at 1-866-953-1530 or email
at doctor@cenegenics.com .
Jeffry S. Life, M.D., Ph.D., is a Diplomate of
the American Board of Family Practice, the American Board of Anti-Aging Medicine, a Fellow of the American Academy of Family
Physicians and is certified in Age Management Medicine. He is a Cenegenics Institute physician and lives a lifestyle that
promotes health and fitness. He writes a column on Performance Nutrition for Muscle Media Magazine and was the Grand Champion
of the Body-for-LIFE Contest in 1998.
Aetna
InteliHealth – featuring Harvard Medical School’s Consumer Health Information
November 30, 2001
Excerpt from “Ask the Expert” on Male Menopause (Andropause)
No Myth
Q: Is there such a thing as “male menopause”?
A:
Yes, there may well be such a thing as male menopause, but the malaise goes far beyond the so-called "midlife crisis" of popular
culture. More specifically, the male version of menopause is the gradual decline in the chief male sex hormone, testosterone,
which in the average man begins as early as the third decade of life. Most men remain unaware of the decline, but researchers
now believe that it may be associated with common age-related changes like high cholesterol, muscle weakness, weight gain,
and heart problems.
Q: Do men undergo something like menopause as
they age?
A: The term "male menopause" is really something of a misnomer. What the average healthy man will experience
as he ages is not a noticeable change, like female menopause, but a gradual decline in the principal male sex hormone, testosterone.
The decrease can begin in the late thirties, and by the seventies, blood levels may have dropped by one-third to one-half
of the levels observed in young men.
We believe that this decline is linked to common age-related changes in healthy
men, such as decreases in muscle tissue and bone mineral density, increases in abdominal body fat, a rise in cholesterol,
and deteriorating heart function, as well as psychological and sexual changes. We know that such hormonal associations with
aging exist for women, and we can treat them with replacement therapy. We also know that young men with severe testosterone
deficiency suffer from muscle weakness, osteoporosis and psychosexual dysfunction, and that these problems lessen or disappear
when such men are given a testosterone supplement.
Q: What research
is currently being done in this area?
A: Three large NIH-funded human trials have recently been completed. The tabulated
data will likely confirm and extend our beliefs about the role of testosterone decline and supplementation in healthy aging
men. We expect some important findings will be published next year that will allow us to look at the aging process differently,
and help us take a kinder, gentler approach to improving older men's quality of life.
Q: Can the decline be treated with hormone replacement, as with postmenopausal women?
A: Smaller studies
have already suggested that very gradually replacing testosterone in selected healthy men can actually reverse some of the
age-related problems of muscle weakness, osteoporosis, high cholesterol and others. For example, it may be beneficial for
some men to begin receiving supplemental therapy while still in their thirties.
Q:
Is there a chance that testosterone supplements could cause prostate disease?
A: Studies suggest that although testosterone
is not a cause of new prostate cancer, it can contribute to the growth of existing prostate cancer. For their safety, men
with this cancer were excluded from all the studies and we carefully and continually screened other participants for any sign
of the disease. However, it's our hypothesis that slow, gentle supplementation to help men return to their previous blood
levels of testosterone is safe for men who are cancer free at the inception of testosterone therapy.
Q: Are there other potential complications of testosterone supplementation?
A: We know
that a man's cholesterol profile can worsen with too much testosterone. However, based on our investigations of men with deficiencies,
we believe that slow, gentle supplementation can actually improve their condition, lowering the bad cholesterol and boosting
the good.
Q: Can elderly men with other age-related illnesses benefit,
or is the therapy limited to the healthy?
A: Elderly men who suffer from co-morbid conditions such as malnutrition,
heart disease and diabetes mellitus also appear to have a more severe decline in testosterone than do healthy men. We believe
they can gain particular benefits from supplementation, and researchers are starting to look at possible usefulness in diverse
frail elderly populations. We hope that the therapy can prolong their independence and improve their quality of life.
|
Testosterone
Therapy in Men: An Update
Laurence Katznelson, M.D., Harvard Medical School
Neuroendocrine Center
Bulletin Vol 6, Issue 2, Winter 2000
|
|
Testosterone deficiency
in men is manifested typically by symptoms of hypogonadism, including decreases in erectile function and libido. Testosterone
also has an important role in the regulation of normal growth, bone metabolism and body composition. Specifically, testosterone
deficiency is an important risk factor for osteoporosis and fractures in men. In men older than 65 years of age, the incidence
of hip fracture is 4-5/1000 and approximately 30% of all hip fractures occur in men. Men with testosterone deficiency have
significant decreases in bone density, particularly in the trabecular bone compartment. Testosterone deficiency has been reported
in over half of elderly men with a history of hip fracture. Men with testosterone deficiency also have alterations in body
composition that include an increase in body fat. Using quantitative CT scans to assess fat distribution, we have shown that
testosterone deficiency is associated with an alteration in site-specific adipose deposition with increased deposits in all
areas, particularly in the subcutaneous and muscle areas. Because truncal fat correlates with glucose intolerance and cardiovascular
risk, hypogonadism may have important implications with regard to overall health and mortality. In one study, the alteration
in skeletal muscle composition was associated with a decrease in muscle strength. Therefore, testosterone deficiency is associated
with an enhanced risk for osteoporosis, altered body composition including increases in truncal fat, and, possibly, decreases
in muscle performance.
Administration of adequate testosterone replacement therapy leads to improvements in libido
and erectile function. Following testosterone replacement, men note an increase in energy and mood, which may reflect either
direct behavioral effects of androgens, and/or, an elevation of hematocrit due to rising testosterone levels. Testosterone
therapy also leads to important beneficial effects on the skeleton and lean tissue mass. Testosterone replacement increases
bone density in hypogonadal men with the most dramatic effects seen in the trabecular bone compartment. These effects may
be seen as early as 6 months following initiation of testosterone therapy. In one recent study of the long-term benefits of
testosterone therapy, the greatest benefits in trabecular bone were seen in the first several years of therapy. With regard
to body composition, testosterone replacement therapy results in a dramatic reduction in adipose content, with the greatest
effects seen in the subcutaneous and skeletal muscle areas. Androgen therapy leads to a significant increase in lean skeletal
muscle mass and strength. Therefore, there are beneficial effects of testosterone replacement on body composition and bone
mineral density in adult hypogonadal men that may serve as indications for therapy in addition to libido and sexual function.
Because
testosterone levels decline with age, and aging is accompanied by body changes including loss of muscle and increases in fat,
there is great interest in the potential benefits of testosterone administration in elderly men. In a recent study, Snyder
et al. (1999) administered testosterone via a scrotal patch in a randomized, placebo-controlled trial to 108 elderly men for
3 years. As shown in Figure 1, testosterone administration resulted in beneficial effects on lean and fat mass. Therefore,
there may be a role for androgens in improving body composition and function in elderly men. |
|
Figure (1). Mean
change from baseline in total body mass, fat mass, and lean mass, as determined by DEXA, in 108 men over 65
yr of age.
The decrease in fat mass (P < 0.005) and the increase in lean mass (P < 0.001) inthetestosterone-
treated subjects were significantly different from those in the placebo-treated subjects at 36 months.
(Reproduced
with permission from The Endocrine Society - Snyder PJ, et al: The Journal of Clinical Endocrinology &
Metabolism 1999; 84:2647-2653). |
Figure 1.
GRAPHS AT BOTTOM OF PAGE
|
References
1. Jenkins et al. Insulin-Like Growth Factor-I and the Development
of Colorectal Neoplasia in Acromegaly. J Clin Endocrinol Metab. 2000. 85:3218-21.
2. Renehan et al. The Prevalence and
Characteristics of Colorectal Neoplasia in Acromegaly. J Clin Endocrinol Metab. 2000. 85:3417-24.
|